The phrase “bionic” conjures sci-fi visions of people enhanced to superhuman ranges. It’s true that engineering advances akin to higher motors and batteries, along with trendy computing, imply that the required mechanical and digital techniques are not a barrier to superior prostheses. However the discipline has struggled to combine these highly effective machines with the human physique.
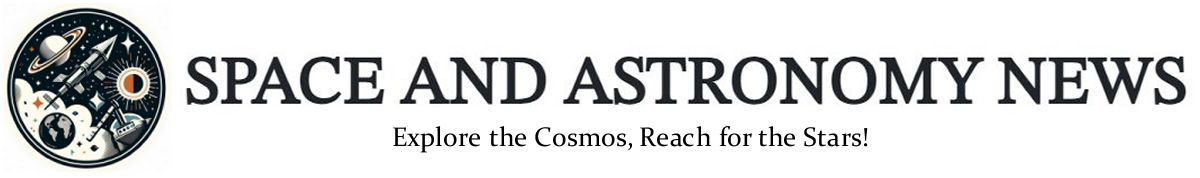
That’s beginning to change. A latest trial examined one new integration method, which entails surgically reconstructing muscle pairs that give recipients a way of the place and motion of a bionic limb. Alerts from these muscle tissue management robotic joints, so the prosthesis is absolutely beneath management of the person’s mind. The system enabled individuals with below-knee amputations to stroll extra naturally and higher navigate slopes, stairs and obstacles, researchers reported within the July Nature Drugs.
Engineers have usually considered biology as a hard and fast limitation to be engineered round, says bioengineer Tyler Clites, who helped develop the method a number of years in the past whereas at MIT. “But when we have a look at the physique as a part of the system to be engineered, in parallel with the machine, the 2 will have the ability to work together higher.”
That view is driving a wave of methods that reengineer the physique to raised combine with the machine. Clites, now at UCLA, calls such methods “anatomics,” to differentiate them from conventional bionics. “The problem we have been tackling wasn’t an engineering drawback,” he says. “The best way the physique had been manipulated in the course of the amputation wasn’t leaving it able to have the ability to management the limbs we have been creating.”
In an anatomics method, bones are exploited to offer secure anchors; nerves are rerouted to create management alerts for robotic limbs or transmit sensory suggestions; muscle tissue are co-opted as organic amplifiers or grafted into place to offer extra sign sources. These methods all enhance the connection and communication between a robotic limb and the human nervous system, enhancing what bionic prostheses are able to (SN: 2/9/24).
Anatomics-based gadgets have been gradual to make their method out of labs and into the industrial and medical worlds. However some say the sphere is edging us nearer to that sci-fi imaginative and prescient of seamlessly built-in, brain-controlled bionic limbs — particularly as extra advances lie across the nook.
Right here’s a better have a look at how researchers are aiming to marry physique and machine.
Reconstructing muscle tissue
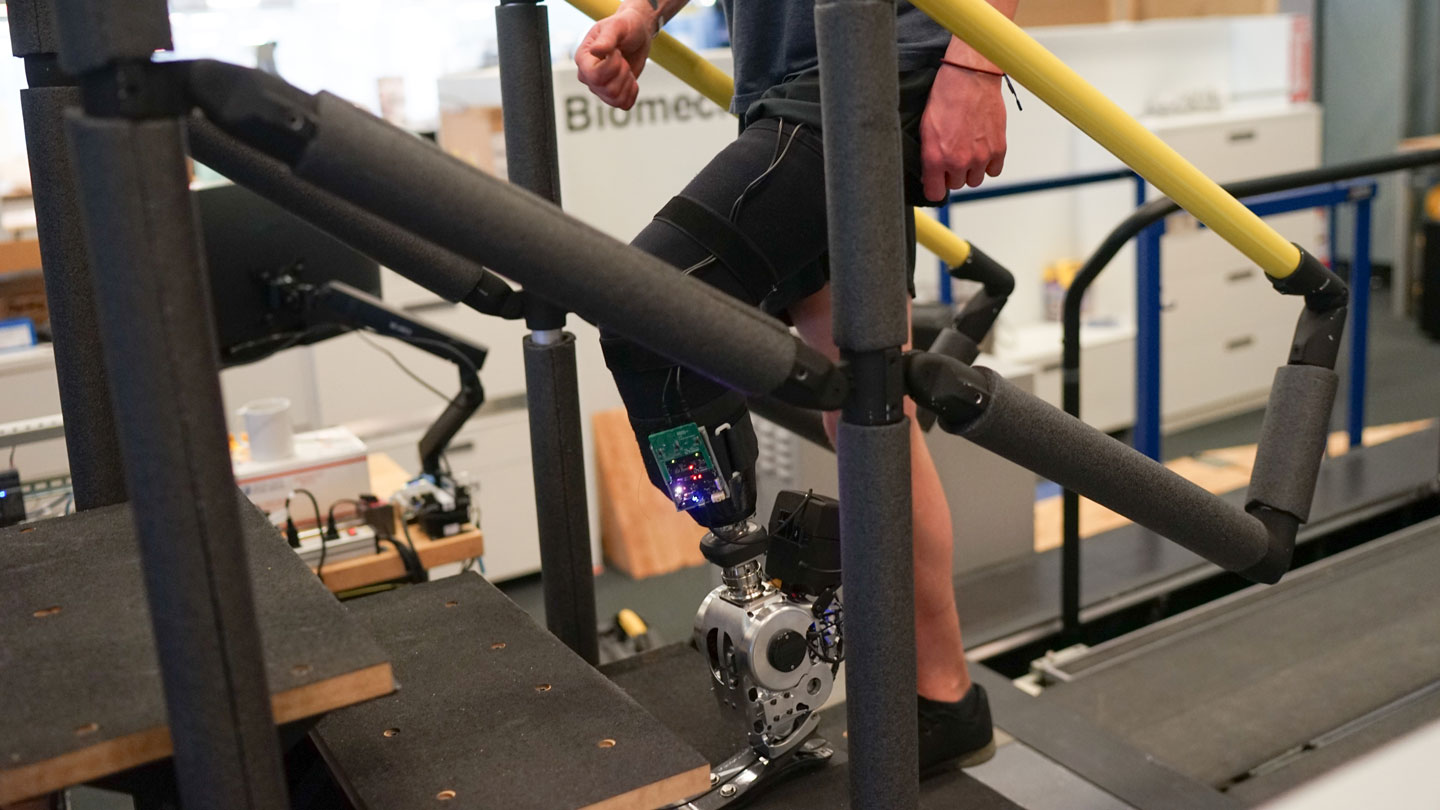
Proprioception — the physique’s consciousness of itself in area — is a tough sense to revive, but it surely’s necessary for motion, particularly strolling (SN: 9/9/19). Muscular tissues ship alerts to our mind about the place our physique is, how it’s transferring and what forces it encounters. These alerts are generated primarily by coupled muscle tissue referred to as agonist-antagonist pairs, the place one contracts as the opposite stretches.
In a conventional amputation, this necessary suggestions is discarded. However the method reported within the July research, generally known as an agonist-antagonist myoneural interface, or AMI, surgically reconstructs these push-pull pairs and makes use of the alerts they generate to manage prosthetic joints. The process allows a recipient to “really feel” their prosthetic limb.
“When the prosthesis strikes, the particular person really feels that motion as a pure proprioceptive sensation,” says MIT bionicist Hugh Herr, who developed the method alongside Clites and the group’s surgeon Matthew Carty.
The latest research was a part of a medical trial that Herr and colleagues are conducting, which examined the method in 14 individuals with below-the-knee amputation. Seven individuals had undergone the AMI process, whereas the others had normal amputations. Recipients of the AMI-based system elevated their strolling velocity by about 40 p.c from 1.26 meters per second to 1.78 meters per second, the researchers discovered, a charge corresponding to that of individuals with out amputation.
Extending bones
The commonest complaints from prosthetic customers contain ache and discomfort. A significant supply of discomfort is the attachment level.
“Most of the issues with prosthetic utilization are associated to the socket,” says bioengineer Cindy Chestek of the College of Michigan in Ann Arbor. Squishy flesh is poorly suited to transferring hundreds to the a part of the physique constructed for that job — bones. The ensuing pressure could cause tissue harm and, invariably, discomfort, generally main customers to desert their machine.
A method referred to as osseointegration exploits the truth that sure metals bond with bone. A titanium bolt inserted into the skeleton anchors the prosthesis in place, offering larger power, stability and luxury. “There’s a cause we have now skeletons,” Chestek says.
The process was first carried out in 1990 however didn’t change into broadly accepted and clinically accessible till the previous decade. One implant system, referred to as OPRA, acquired approval from the U.S. Meals and Drug Administration in 2020. The primary downside is that the titanium bolt should undergo the pores and skin, making a everlasting gap that carries an infection dangers. “Apart from the an infection threat, osseointegration is best in all methods,” Chestek says.
Rerouting nerves
Bionicists have lengthy sought to faucet into the physique’s nerves to create prostheses that talk with the mind. However early efforts have been irritating, primarily as a result of the alerts that nerves carry are very weak.
“Individuals tried for many years to get significant alerts from [putting] a wire inside a nerve,” Chestek says. “To today, it’s practically unattainable exterior of a managed lab setting.”
Trendy bionic prostheses talk largely with muscle tissue as a substitute. When activated by a nerve, muscle tissue emit a lot bigger electrical alerts, which will be picked up by electrodes on the pores and skin, which then management the prosthetic limb.
However nerves that beforehand operated elements of a lacking limb — and will equally effectively function the substitute limb — don’t often finish in muscle tissue. They go nowhere, which creates neuromas, bulbs at nerve ends whose electrical “sparking” causes ache.
A process referred to as focused muscle reinnervation, or TMR, solves this drawback. A surgeon strips muscle tissue of their native nerves and reroutes severed nerves to this freshly cleared floor. Rerouted nerves develop into the muscle tissue over time, which act as amplifiers, creating sources of the required management alerts. “You flip a nerve recording drawback right into a muscle recording drawback,” Chestek says. “Muscle recording is straightforward.” The process additionally treats neuroma ache — a function for which it’s usually carried out.
A downside is that TMR cannibalizes present muscle tissue, limiting the variety of alerts that may be created. “You run out of actual property fairly rapidly,” Chestek says. That is particularly necessary for amputations above the knee or elbow, the place there are fewer remaining muscle tissue and extra prosthetic joints to manage.
A brand new method, generally known as a regenerative peripheral nerve interface, or RPNI, surgically inserts small muscle grafts taken from elsewhere and reroutes nerves to those as a substitute. Surgeons can then dissect these nerve bundles into their constituent fibers to capitalize on the newly grafted targets, permitting researchers to create as many alerts as they want, Chestek says.
The small dimension of the muscle grafts makes it troublesome to choose up alerts from them utilizing floor electrodes, although. “You may’t report [electrical signals] from a three-centimeter piece of muscle by the pores and skin very simply,” Chestek says. “You must use implanted electrodes.” That is extra invasive, and implants face regulatory hurdles, however implanted electrodes produce increased high quality alerts. They simply must be accessed someway, as operating wires by the pores and skin isn’t viable exterior of laboratory research.
Some researchers are engaged on wi-fi techniques, however one other resolution is to mix RPNIs with osseointegration. On this setup, wires between implanted electrodes and the prosthesis merely run by the titanium bolt. A research printed final yr described an above-the-elbow bionic arm utilizing this method that enabled the recipient to manage each finger of his robotic hand.
Rebuilding our bodies
At his UCLA anatomics lab, Clites says, “I’ve received 9 or 10 lively collaborations with surgeons on totally different tasks.” Right here, he and his group use cadavers to check concepts and collect knowledge. “We’ll mount cadaver limbs to a manipulator arm and consider the techniques we’re creating to verify they work as supposed,” Clites says. “It’s the spine of what we do.”
One of many tasks beneath improvement is a brand new attachment technique that avoids the everlasting gap that comes with osseointegration. As a substitute of a titanium bolt, there’s a bit of metal within the limb and an electromagnet within the socket of the prosthetic. “That magnet holds [the socket] onto the limb,” Clites says, “after which you’ll be able to management how a lot engaging pressure there’s by altering the present by that electromagnet.” The socket doesn’t should bear hundreds; the magnetic pressure does that job, altering from second to second in accordance with necessities, akin to strolling versus standing.

At MIT, Herr can be engaged on a brand new advance. The latest trial of AMI-based bionic legs used electrodes on the pores and skin to shepherd alerts from muscle tissue to the prosthetic joints. However floor electrodes have drawbacks, akin to motion inflicting sign distortions. The brand new method — referred to as magnetomicrometry — entails putting magnetic spheres inside muscle tissue and monitoring their motion with magnetometers. “With these magnets,” Herr says, “we are able to measure what we care about and use it to straight management the bionic prosthesis.” A industrial product will exist in about 5 years, he says.
For Herr, such advances are private. Each of his legs have been amputated under the knee after a mountaineering accident 42 years in the past. He’s considering of upgrading to AMI-based bionic leg prostheses within the coming years. As soon as these methods are perfected, he predicts a leap ahead. “Once you marry surgical methods like AMI and RPNI with one thing like magnetomicrometry, we imagine it’s going to be sport over,” Herr says. “We imagine there’s going to be the Hollywood model of brain-controlled robotic limbs.”
An added good thing about restoring proprioception, alongside other forms of sensory suggestions akin to contact, is that it makes recipients really feel extra like a prosthetic is a part of themselves (SN: 4/22/21). “The aim within the discipline is after we do robotic reconstruction, the particular person says, ‘Oh my God, you’ve given me my physique again.’” Herr says. “As a substitute of a robotic instrument, we give them a complete limb again. The sector may be very near that aim.”
*
Supply hyperlink

No comments! Be the first commenter?